What is Prolapse?
When the supportive tissues covering a part of the body weaken or stretch, occurs a bulge, dropping the organ down. This movement of the organ out of its original place is known as Prolapse. There are several types of prolapse, namely,
- Pelvic Prolapse
- Rectal Prolapse
Everything You Need to Know About Prolapse
What is Pelvic Organ Prolapse?
The pelvic organ prolapse means when the organs forming a cover or floor to the pelvic area, drop down. Most women are affected by this. The muscles surrounding the pelvic organs hold them in the right place but due to some problems, they might undergo flexing and stretching. Pelvic organs include – rectum, vagina, and uterus.
If there is a pelvic floor disorder then one or more of these organs might stop working properly. There are certain effects of pelvic floor disorder, which include pelvic organ prolapse, urinary inconsistency, and anal problems.
When the pelvic organs come down into or outside the anus or vaginal canal, it is given the following names
- Uterine prolapse
- Urethrocele
- Vaginal prolapse
- Cystocele
- Enterocele
- Rectocele
Why does prolapse occur?
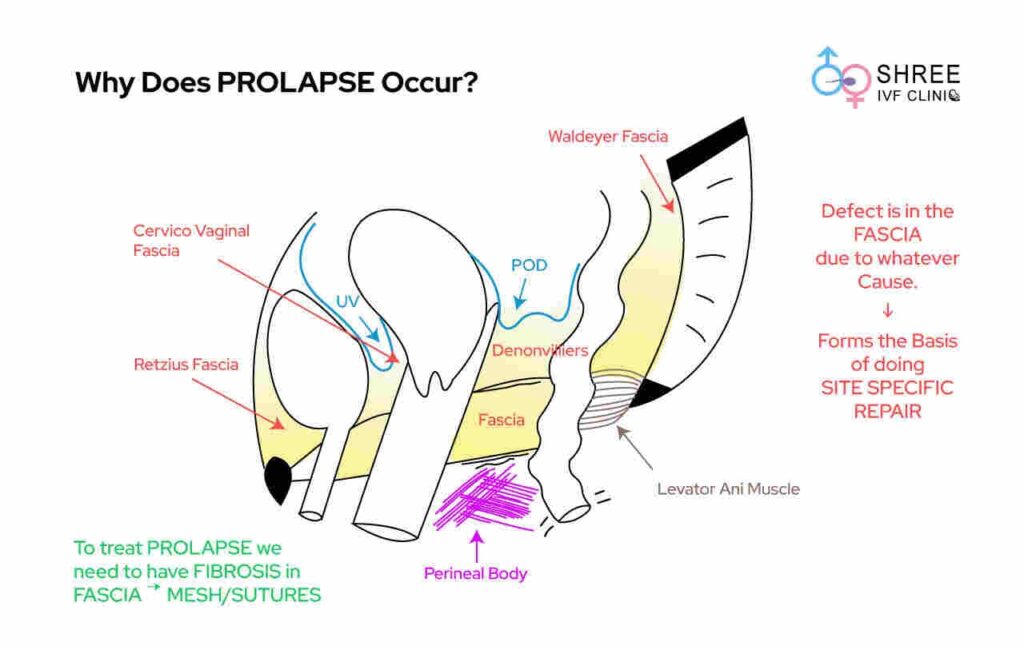
Pelvic organ prolapse is extremely commonly seen in India. Though it is commonly associated with birth trauma especially due to prolonged labour and normal vaginal delivery, this disease is also seen in women who are in the post-menopausal age group. In India malnutrition also significantly contributes to a higher risk of prolapse.
Prolapse predominantly occurs due to a defect in the endopelvic fascia. The endopelvic fascia keeps all the pelvic organs bound to each other. It consists of collagen and other fibroblasts and is predominantly strengthened and acted upon by oestrogen.
In cases of oestrogen deficiency which is predominantly seen in postmenopausal women the endo pelvic fascia undergoes defects, which results in the development of pelvic organ prolapse.
Uterine Prolapse Stages
Let us first categorize the four stages of pelvic organ prolapse:
- Stage I – The uterus will be in the upper half of the vagina
- Stage II – It will also descend to the opening of the vagina
- Stage III – It pokes out of the vagina
- Stage IV – It will come out of the vagina completely
Symptoms of Pelvic Prolapse
It is hard to notice any symptom in particular. The symptoms are not universal i.e. they vary according to the organ affected. If you remain very careful then you may notice the possible signs.
- Lower back pain
- Pain during sexual intercourse
- Constipation
- Feeling unnecessary pressure in the pelvic area
- Problems related to urination
- Problems like blood clotting or spotting during menstruation
Very early stages of stress urine incontinence especially where it is associated only with leakage of very small drops causing just wetness in the vagina can be treated with the help of Kegel exercise.
This typically involves controlled supervision under a physiotherapist which helps in specific strengthening and contraction of pelvic floor muscles which in fact after 3 to 4 months of therapy may help in better control of the urine leak in early stages in social circumstances.
For any form of advanced-stage disease where there is a severe leakage of urine even on the lightest of the activity performing any form of pelvic strengthening is definitely going to have no benefit as a curative therapy for stress urine incontinence.
Causes of Pelvic Organ Prolapse
Urinary incontinence can be temporarily caused by urinary tract infections, which are extremely commonly seen in India.
This requires infection-specific treatment. It normally takes 2 to 4 weeks for it to subside. This may require the patient to take a specific course of antibiotics after urine culture.
Clinical examination of urine leak on a partly filled bladder or a full bladder is one of the best methods to diagnose this condition.
If it is also associated with mixed or urge incontinence, then one may choose to do a urodynamic study.
There are a few specified causes, like,
- Hysterectomy (removal of the uterus through surgery)
- Cancer in the pelvic organs that causes constant disturbance in the abdominal area.
- Obesity can be one of the major reasons your body encounters flexing and stretching or fat formation in the pelvic area.
- Long-term problems related to coughing can put excessive pressure on your lower abdomen, leading to loosening of the muscles.
- Weaker tissues connecting the organs
- Chronic constipation
- Giving birth at a young age because the body parts are not yet ready.
What are the different types of Prolapse?
Anterior compartment, apical compartment and posterior compartment. These are the three main locations where one can focus for examination and classification of pelvic organ prolapse.
However typically this is usually a global prolapse when done in a clinical setting. Anterior compartment descent is also called as Cystoscoele, posterior compartment descent is also called as rectocele.
How is the diagnosis made for Pelvic Organ Prolapse?
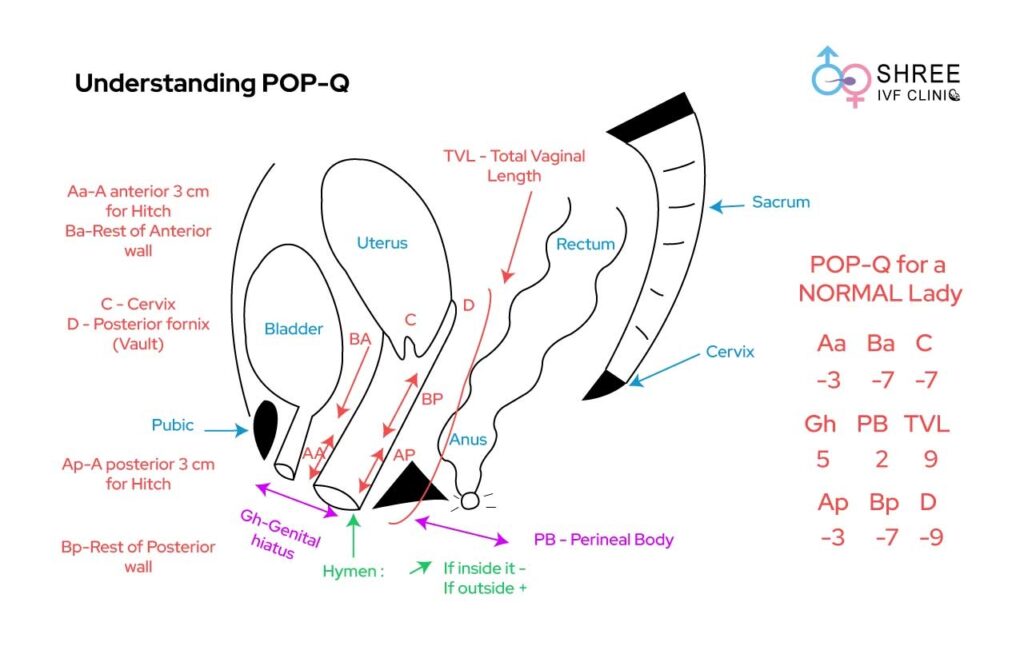
This is predominantly diagnosed on clinical examination. The examination involves a predictive score of something called POP-Q (Pelvic Organ Prolapse Quantification) system. This allows for accurate mapping of the degree of prolapse.
Simultaneous examination of the patient is also done with a partly filled bladder in order to rule out any form of incontinence.
Pay a Visit to Doctor
If you see any of these signs then there is surely some trouble. So it should be a call enough to visit a doctor. Your doctor may suggest some more tests to find out the real deal.
- CT scan of the pelvis
- Ultrasound of the pelvis
- X-ray of the urinary tract
- Magnetic Resonance Imaging (MRI) is suggested
Expectations After Surgery
You can expect a smooth life after surgery. It will solve problems related to pregnancy and other major issues. Doctors advise undergoing the treatment as a permanent solution.
Restrictions after prolapse surgery and Recovery
- Driving
- Heavy exercise
The drip is removed after twenty-four hours. There might be some bleeding in the vagina which can be prevented by using gauze. It is removed only when the bleeding stops. Doctors advise resting for a minimum of three to five weeks. After that, you can be back to a normal lifestyle.
Lifestyle Changes After Surgery
Your main focus should be on maintaining a proper diet as constipation is common. You should drink a lot of water. Healthy eating like fruits and vegetables can cause you a speedy recovery.
People usually think reducing water intake help in treatment of Stress Urine Incontinence. But reducing the water intake can increase the chances of having urinary tract infection.
Even if a woman is experiencing urine incontinence it is not advisable for them to reduce their water intake. Staying well hydrated is extremely important for maintenance of good health of the urinary bladder.
Early stages of stress urinary incontinence, where the leakage is minimal and causes only vaginal wetness, can often be treated with Kegel exercises.
You should avoid doing anything that would put pressure on your pelvic area. You can rely on laxatives and gentle exercises only with the permission of your doctor.
The problem may seem to be a major one, but once you decide to face it, you get a solution. You need a positive mindset to fight such diseases.
FAQ’s
– How does a lady come to know that she is having a prolapse?
Predominantly a lady would complain of something coming down from the vagina or out from the vagina. This is typically associated with urinary tract infections or constipation or slightly altered bowel motility.
In rare occasions the entire pelvis organs can prolapse outside which is also called as procidentia. Sometimes this can also present with vaginal bleeding especially if there is presence of an ulcer in the region of the prolapse.
– Which is the Strongest support to the Uterus?
The apical support which is also called as the level 1 support is the strongest support to the uterus; it predominantly consists of a dense network of fascia which is found around the Pericervical ring.
– Are there complications of the Mesh placement in prolapse?
No, when placed correctly mesh is an extremely good device in order to support the endo pelvic fascia so that the chances of recurrence of prolapse are drastically reduced. Mesh related complications are predominantly due to an incorrect surgical technique.
Laparoscopic surgery for prolapse repair requires an extremely good surgical technique where one has to detect in between the two layers of the endo pelvic fascia. And then anchor the mesh correctly in between that space.
– Does the surgery for prolapse repair have any long term complications?
The patients are required to follow up in the hospital once a year for the next 3 years. Long term complications if the surgical technique is correct or virtually next to zero
– When can a patient begin activity after this surgery?
Patients are encouraged to get back to work including weightlifting, working on the farm, doing all household work as well as going to the office within 3 to 4 days of surgery.
– Is uterus removal mandatory in Prolapse Surgery?
There are many young women who are yet to get married or even get to become pregnant who experience pelvic organ prolapse. Hysterectomy for uterus removal has virtually no role in the surgery for prolapse repair. However in postmenopausal women the option to remove the uterus simultaneously is always given to them.
Removal or conservation of the uterus does not increase or decrease the complexity of the surgery as well as the post operative outcome as well as the long term out term of the patient in any manner.
– Can a patient become pregnant after Prolapse Repair Surgery?
Young women who undergo prolapse repair surgery and pelvic reconstruction can easily plan for pregnancy within 3 months of the surgery. Most of this payment has an absolutely uneventful outcome during pregnancy, and can have absolutely normal and healthy children. In young women having pelvic organ prolapse is one of the most important causes of having infertility as well. Infra vaginal elongation of the cervix, is commonly seen in young women.